Medical Software Development: Definition, Types, Benefits, Technologies, Phases, and Features

Healthcare software development is the process of designing, building, managing and scaling software that is used for medical tasks or supports healthcare facility services. It includes various types of applications that are used in diverse operations and scenarios. Get valuable insights into healthcare software development in this in-depth guide.
The healthcare industry is evolving rapidly, with technology becoming a core part of this shift. Whether it’s hospital management software systems, wearable devices, or more complex, specialized applications, the adoption of technology is widespread to meet modern healthcare needs. This is reflected in various software that help secure competitive advantage.
As a result, the global healthcare software-as-a-service (SaaS) market, valued at $28.66 billion in 2022, is projected to hit $77.43 billion by 2032.
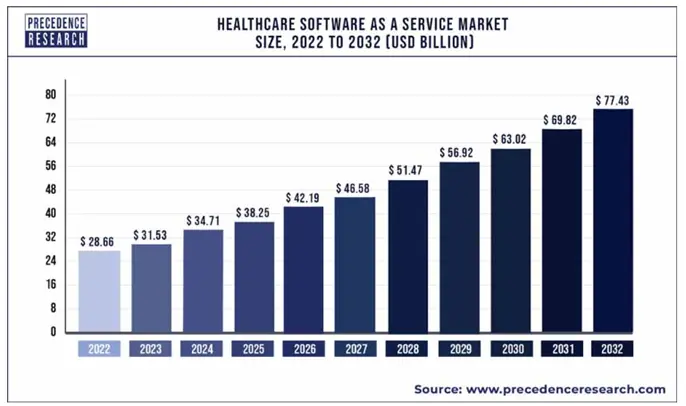
Source: Precedence Research
Healthcare businesses are pouring resources into digital investments for bringing improvements in the delivery of healthcare services. As per Deloitte, 88% of them are focused on enhancing patient experience, 68% into clinical care delivery, and 80% channeling investments into cybersecurity and IT.
One key factor that distinguishes medical and healthcare software development is that the process has to be executed within the confines of strict regulatory boundaries. However, with the right approach to software development, businesses can address these key areas efficiently.
Considering all these complexities, we cover all its nuances and provide a comprehensive roadmap for anyone looking to understand and succeed in the development of medical and healthcare applications.
What is Medical Software?
A medical software is a suite of programs that perform tasks associated with various processes in healthcare operations. It can also be seen as an umbrella term for various software applications designed to manage or streamline various processes in the healthcare value chain. For instance, a medical application simplifies clinical workflows, aids in efficient management of patient information, and supports decision-making.
Types of Medical Software
Based on the application within the healthcare space, medical application development follows different trajectories decided by the area-specific processes and the compliances involved. Majorly, it revolves around the development of:
- Electronic Health Records (EHR) Systems
- Practice Management Software
- Medical Billing Software
- Clinical Decision Support Systems (CDSS)
- Telemedicine Software
- Personal Health Record (PHR) Systems
- Medical Imaging Software
- Laboratory Information Management Systems (LIMS)
- Mobile Health Apps
- ePrescribing Software
Managing patient data has always been a cornerstone of healthcare, and EHR systems have become the go-to solution for organizing this information. Designed to store, retrieve, and share medical records, these systems rely on structured databases to keep everything in order.
They also adopt standardized frameworks like HL7 and FHIR, which allow different healthcare systems to exchange information. EHRs replace outdated paper-based methods, addressing inefficiencies in data sharing and reducing the risk of errors. By facilitating secure access to comprehensive patient histories, they support more accurate diagnoses and better treatment plans.
Administrative tasks in healthcare settings, such as appointment scheduling and billing, have historically been a source of bottlenecks. Practice management software tackles these issues by centralizing operations.
Equipped with features to manage schedules, process insurance claims, and organize patient records, these tools reduce the workload on staff. Integration with standardized billing codes like ICD-10 and CPT makes financial processes more transparent and accurate. This software not only minimizes administrative headaches but also supports a smoother experience for both providers and patients.
Billing errors and delays in reimbursement have long plagued the healthcare sector. Medical billing software addresses these issues by automating the claims process. Using coding standards such as ICD-10, CPT, and HCPCS, the software ensures precision in claim generation.
The software connects directly with clearinghouses to validate claims, reducing the likelihood of rejections. This efficiency is pivotal in maintaining cash flow for healthcare providers while offering transparency to patients regarding their medical costs.
Decisions in healthcare carry high stakes, and CDSS has stepped in to make them more informed. These systems analyze patient data alongside established clinical guidelines to provide evidence-based recommendations.
By integrating with EHRs, they deliver real-time alerts about potential drug interactions, allergies, or missed diagnoses. Traditional reliance on manual research and memory is replaced with a technology-driven approach, reducing the risk of oversight. CDSS tools empower clinicians to make decisions backed by data, ultimately improving patient safety.
Access to healthcare services has been a persistent issue, particularly for those in remote areas. Telemedicine platforms bring medical consultations to patients through real-time communication tools.
Using protocols like WebRTC, telemedicine tools enable video calls, voice chats, and secure messaging between doctors and patients. Encryption methods ensure the confidentiality of sensitive health data. These platforms break geographical barriers and make healthcare more accessible, offering convenience without compromising the quality of care.
Patients today expect greater control over their health information, and PHR systems make that possible. These tools let individuals access and manage their medical records, including lab results and prescriptions.
PHR systems pull data from EHR systems and provide a consolidated view of a person’s health history. Traditional practices left patients disconnected from their own information, but PHR systems fill that gap. Empowering individuals with easy access to their records promotes engagement in their healthcare decisions.
Interpreting medical images like MRIs and CT scans is a complex task, made more manageable by specialized imaging software. These tools support the storage, transmission, and analysis of high-resolution images, adhering to standards like DICOM.
Large file sizes, a traditional challenge in medical imaging, are handled efficiently with advanced compression techniques. With GPU-accelerated processing, the software speeds up the rendering of images, allowing radiologists to analyze them more quickly and accurately.
Managing samples and test results is a meticulous process in laboratories, often prone to errors. LIMS automates workflows, organizes data, and keeps detailed audit trails for compliance purposes.
Features like barcode scanning and RFID integration bring precision to sample tracking. With these features, the software transforms laboratory operations, replacing manual processes with a system that keeps everything organized and traceable.
People are increasingly relying on smartphones to monitor their health, as mobility continues to revolutionize healthcare. Mobile health apps collect data from wearable devices, facilitate communication with healthcare providers, and store information securely in the cloud.
Mobile apps that work on both iOS and Android platforms ensure widespread adoption. Such apps are a key lever of digital transformation in healthcare. Traditional barriers like limited access to personal health data are removed, giving patients a direct line to monitor and manage their health.
Handwritten prescriptions have historically been a source of confusion and errors. ePrescribing software eliminates these challenges by enabling electronic transmission of prescriptions. It incorporates standards like NCPDP SCRIPT to align with pharmacies and healthcare systems.
Features such as automatic checks for drug interactions and dosage guidance bring an additional layer of safety. Compliant with DEA regulations, this software supports controlled substance prescriptions while reducing the chances of mistakes.
Benefits of Developing Software for Medical Facility
Software development brings transformative advantages that reshape healthcare delivery and streamline operations across the healthcare industry. The benefits include improved patient care, enhanced healthcare delivery, better data management, reduced costs, streamlining of admin processes, better data-based decisions, and better compliance. We discuss them at length below:
- Advanced Care and Patient Safety
- Smarter Workflows
- Accessible and Accurate Data
- Cost-Effective Operations
- Smoother Administrative Workflows
- Data-Driven Health Decisions
- Staying Ahead with Regulations
Medical software relies on cutting-edge algorithms to assess clinical data, spotting potential health risks before they escalate. For instance, applications that detect early signs of sepsis in hospitalized patients have drastically reduced mortality rates. Early interventions like these transform healthcare delivery into a proactive service.
Repetitive chores like updating patient records or scheduling appointments are time-consuming and prone to errors. Automation tools take over these responsibilities, freeing up healthcare staff to devote more attention to what really matters—providing quality care. For example, digital scribing tools now handle documentation, allowing doctors to focus during consultations.
Healthcare ecosystems thrive when data flows without interruption. Protocols such as FHIR bridge gaps between systems, making patient histories instantly available. A practical example is emergency rooms accessing a patient’s allergy records in real time, preventing life-threatening medication errors.
Shifting infrastructure to the cloud has revolutionized how healthcare facilities manage expenses. Gone are the days of investing heavily in hardware and dedicated IT staff. Hospitals now allocate their budgets more effectively, using subscription-based models to access advanced software solutions.
Revenue cycle management systems are reshaping administrative tasks in healthcare. By analyzing patterns in claims data, they significantly cut down denials and reduce delays in reimbursement. For instance, predictive analytics can identify coding errors in real-time, preventing revenue loss.
Data analytics shines brightest in helping businesses stay aligned with the latest trends as well as gear up to combat potential risks. By pinpointing at-risk groups, healthcare providers roll out targeted programs, leading to noticeable improvements in public health. A great example is analyzing geographic data to combat outbreaks of infectious diseases more efficiently.
Regulatory compliance is no longer a guessing game. Medical software meticulously tracks changes in healthcare laws, ensuring organizations adhere to requirements. For example, tools that align electronic health records with HIPAA guidelines minimize liability and avoid hefty fines.
Challenges in Medical and Healthcare Application Development
Custom software development in the healthcare landscape comes with its own set of challenges – both technical and business – as we discuss below.
- Older healthcare systems are notoriously hard to integrate with, due to outdated architecture and lack of standard APIs.
- Medical algorithms, like those used in diagnostics, require extremely high accuracy and even a small error in calculations can have serious consequences.
- The sheer amount of medical data—combined with strict privacy regulations—creates storage and processing difficulties.
- Healthcare professionals need software that’s easy to use, but medical applications involve complex data and functionality.
- Medical data can be inconsistent at times, since it flows in from various sources with different formats.
Modern Technologies in Medical and Healthcare Development
Building medical software calls for a blend of different technologies, each contributing to various healthcare areas and supporting the development of diverse medical applications. The following are the leading technologies you need in this space:
- Artificial Intelligence and Machine Learning
- Internet of Things (IoT)
- Blockchain Technology
- Cloud Computing
- Big Data Analytics
- Augmented Reality (AR) and Virtual Reality (VR)
- Wearable Technology
- Natural Language Processing (NLP)
One of the foremost healthcare technology trends, AI and ML have reshaped the way healthcare operates by providing tools that reduce errors and elevate the standard of care. These technologies help predict disease patterns, automate administrative tasks, and personalize treatment plans. By analyzing massive datasets, they uncover insights that would otherwise take months to identify. For instance, IBM Watson leverages AI to analyze medical records and recommend treatment options, enabling physicians to make quicker, more informed decisions.
The healthcare industry has embraced IoT to enable continuous patient monitoring and proactive care. Connected devices like smart insulin pens and heart rate monitors transmit real-time health metrics to care providers. This approach helps medical teams intervene swiftly during emergencies. Smart blood pressure monitors, for example, allow doctors to track patient health remotely and react promptly if an anomaly is detected.
Securing sensitive patient data is one of the biggest challenges in healthcare, and blockchain is providing robust solutions. Beyond safeguarding medical records, blockchain is helping track the authenticity of medications from production to distribution. Companies like Chronicled use this technology to authenticate drugs and prevent counterfeit medicines from entering the supply chain, which directly impacts patient safety.
Data management has become more flexible and accessible in healthcare. Thanks to cloud computing and various service models it offers. Hospitals now store patient records on platforms like Microsoft Azure, which allows healthcare teams to access these files regardless of their location. This accessibility not only facilitates better communication among care providers but also supports faster decision-making during treatments.
Healthcare providers rely on big data to draw meaningful insights from the massive amount of patient information they collect daily. Analyzing this data helps them predict disease outbreaks, optimize staffing, and manage resources effectively. For example, analyzing admission trends enables hospitals to allocate beds and supplies more effectively, leading to better preparedness during busy seasons.
Medical training has reached new heights with AR and VR, providing immersive learning experiences that traditional methods lack. Surgeons use these tools to practice intricate procedures, gaining confidence before operating on patients. Osso VR offers virtual simulations where medical professionals refine their techniques, ensuring precision and improving outcomes in actual surgeries.
The demand for health monitoring has skyrocketed, and wearable technology is at the forefront. Devices like smartwatches track essential metrics such as blood oxygen levels and sleep patterns, giving users actionable insights into their well-being. Physicians also benefit as these wearables provide accurate and continuous data, aiding in diagnosing and managing chronic conditions.
Handling healthcare documentation has always been time-consuming, but NLP is changing that. Advanced systems process spoken or written language to assist medical professionals in maintaining accurate records. There are tools that transcribe physicians’ spoken notes, freeing up time for them to engage more with their patients rather than paperwork.
Cost of Developing Medical Software
Let’s discuss the software development cost in detail by covering various factors that influence it, the estimates for various categories we discussed earlier, how to carry out the budget and financial planning, and what are the strategies to adopt for saving costs.
-
Factors influencing the cost
-
Cost estimation for different types of Medical Applications
-
Budgeting and Financial planning for developing Medical Applications
-
Cost-saving strategies
Key elements that impact the cost of software development for healthcare and medical services are:
-
Complexity: Simple apps like appointment schedulers cost less, while complex systems like EHR platforms require more resources and expertise.
Features: Basic features are standard, but advanced functionalities like telehealth add development time and labor costs.
Compliance Requirements: Adhering to regulations increases costs, influenced by expert consultation fees and the extent of compliance needed.
Development Team Location: Outsourcing to software development teams in countries like India or Romania offers cost advantages compared to US-based teams.
The costs for main types of healthcare software are as mentioned below. It’s important to note that these are just estimates. Actual costs will vary widely based on factors we saw above as those will decide the actual development effort required:
|
Type of Medical Software |
Estimated Cost Range |
|
Electronic Health Record (EHR) Systems |
$100,000 – $500,000 |
|
Practice Management Software |
$50,000 – $300,000 |
|
Medical Billing Software |
$30,000 – $200,000 |
|
Clinical Decision Support Systems (CDSS) |
$100,000 – $600,000 |
|
Telemedicine Software |
$75,000 – $400,000 |
|
Personal Health Record (PHR) Systems |
$40,000 – $250,000 |
|
Medical Imaging Software |
$150,000 – $700,000 |
|
Laboratory Information Management Systems (LIMS) |
$100,000 – $500,000 |
|
Mobile Health Apps |
$50,000 – $300,000 |
Follow this strategic approach for effective budgeting and financial planning for software development projects in healthcare:

Follow Detailed Cost Breakdown: Itemize costs into categories like development, design, testing, and deployment, including ongoing expenses for software maintenance and updates.
Allocate Resources Wisely: Identify necessary human resources and skills for each development phase to make informed hiring or outsourcing decisions.
Set Contingency Funds: Allocate a portion of the budget for unexpected costs, particularly for regulatory changes and technology shifts in healthcare.
Consider Development Timelines: Longer timelines increase costs. A clear timeline helps allocate resources efficiently and avoid delays.
Evaluate ROI: Assess the potential return on investment to justify expenses and guide financial planning.
These are two powerful strategies that have been helping businesses optimize the cost of software development. Understand why they must be adopted.
Outsourcing: Partner with a third-party firm specializing in medical software from regions with lower labor cost for substantial savings.
Using Pre-built Modules: Integrate pre-built modules for features like user authentication reduces development time and costs so that resources can focus on customizations rather than building from scratch.
Who are the Key Stakeholders Involved in Building Medical Applications
The following are the stakeholders that collaborate with each other during the entire healthcare app development process so that the process executes as per the plan and delivers the best outcomes.
- Developers: They design and develop the software, thus turning clinical requirements into practical software solutions that are capable of handling everything.
- Healthcare Professionals: They are domain experts who provide input on the software’s usability and functionality, so that it fits seamlessly into medical workflows and enhances patient care.
- Regulatory bodies: They are professional organizations like the FDA which review the software to confirm it meets safety and legal standards before it can be used in healthcare settings.
Medical Software Development Life Cycle (SDLC)
The process of developing medical applications follows a series of stages, which take a medical application from idea to final form. Let’s understand how this cycle works and how it translates the concept into reality.
Requirement Gathering and Analysis
Collaborate with healthcare and medical professionals, patients, and regulatory bodies to identify specific needs. Document clinical workflows, compliance requirements, and usability aspects to guide the software development process effectively.
System Design
Create a user-centered software architecture to accommodate user requirements as well as stipulated healthcare data standards (e.g., HL7, FHIR) . Design user interfaces tailored for clinicians and patients, promoting intuitive interactions and efficient data entry for clinical tasks.
Development and Coding
Write secure, scalable code that adheres to healthcare regulations. Implement strong data encryption and access controls. Document the codebase to support future updates and assist with regulatory audits.
Testing
Conduct thorough testing, including functional checks for patient data management and integration tests with existing healthcare systems. Perform user acceptance testing with healthcare staff to validate usability in clinical scenarios.
Deployment and Implementation
Launch the software in clinical settings, aiming for minimal disruption. Provide role-specific training for users such as doctors and nurses, and monitor the rollout closely during the transition phase.
Maintenance and Support
Continuously track software performance and user feedback within clinical practices. Address bugs promptly and offer ongoing support, while adapting to evolving healthcare regulations and standards.
Carry Out Iterative Improvement and Updates
Regularly collect user feedback to identify areas for development. Implement updates that improve features and usability, adopting an iterative approach that keeps the software aligned with changing healthcare demands.
What are the Must Have Features in Medical Software
Medical application development includes a range of specialized features designed to support healthcare providers. Below, we present important features that are offered in a comprehensive medical applications:
- DICOM and PACS Integration: Supports storing, transmitting, and viewing of medical imaging files like MRI and CT scans.
- HL7 Integration: Assists in the exchange of clinical and administrative data between healthcare systems like EHRs and laboratory information systems.
- ICD-10 and CPT Coding Systems: Built-in support for medical coding standards like ICD-10 and CPT for accurate documentation of diagnoses and procedures.
- eMAR (Electronic Medication Administration Record): Tracks medication administration within healthcare settings, reducing errors and ensuring correct dosages.
- FHIR Compatibility: Integration helps faster data exchange and improved interoperability across healthcare systems.
- Clinical Trials Management: Assists in managing clinical trial data, patient recruitment, and study protocols in research institutions and hospitals.
- Drug Interaction Alerts: Offers real-time alerts for drug interactions, allergies, or contraindications for patient safety when prescribing medications.
- eConsent: Helps healthcare providers in digital consent management for obtaining patient consent electronically, with legal compliance tracking.
- Chronic Disease Management: Offers tools for monitoring and managing chronic conditions like diabetes and COPD, integrated with wearable medical devices.
- RIS and PACS Integration: Allows management of radiology workflows, including scheduling and interpreting diagnostic images, integrated with PACS for image storage.
- Electronic Clinical Quality Measures (eCQM): These are tools that automatically capture and report clinical quality measures to improve patient care and compliance.
- Genomic Data Analysis: Aids in the integration of genomic sequencing data for personalized medicine, aiding in genetic diagnosis and treatment.
- EHR/EMR Integration with Wearables: Allows real-time integration with wearable devices to gather patient data and monitor ongoing conditions.
- Compliance with FDA 21 CFR Part 11: Provides support for electronic records and signatures that meet FDA regulations for pharmaceutical and clinical research software.
- Voice Recognition and Dictation: Offers integrated voice-to-text features for faster and more accurate clinical documentation.
- Real-time Clinical Monitoring (RTCM): Tracks patient vitals in real time during critical care situations.
Best Practices To Follow
Developing medical application requires a solid grasp of both technical precision and healthcare-specific regulations. Healthcare businesses must focus on building software solutions that address the unique needs while adhering to strict regulatory standards. Below are best practices that keep these factors in mind:
- Integrate privacy and security measures from the start, with strong encryption and regular audits to maintain compliance.
- Utilize HL7 and FHIR standards for seamless data exchange between healthcare systems, enabling integration with EHR platforms.
- Conduct comprehensive testing, including unit and integration tests, to ensure reliability and compliance with regulations.
- Log all user actions with timestamps and user IDs, creating a secure and tamper-proof audit trail.
- Involve healthcare professionals in the design process to create intuitive interfaces that streamline workflows.
- Manage live data streams efficiently, minimizing latency, and ensure timely alerts for critical events.
- Build software with a modular design for easier updates and scalability, using microservices for independent component management.
- Perform thorough hazard analysis and implement backup systems and error-checking algorithms to mitigate risks.
- Incorporate AI techniques that provide clear explanations for diagnostic recommendations to build trust among users.
- Establish remote monitoring and timely updates to address vulnerabilities and improve functionality post-launch.
- Maintain clear version control to efficiently manage updates and rollbacks when needed.
- Document decisions, changes, and testing outcomes to facilitate compliance and maintenance.
- Provide thorough training for healthcare professionals to ensure effective software adoption and use.
- Implement multi-factor authentication and regular vulnerability assessments to safeguard against threats.
- Encourage collaboration among developers, clinicians, and compliance experts for holistic healthcare software solutions.
Seek Professional Medical Software Development Services From Finoit
Choosing Finoit as your development partner for your medical and healthcare software development project sets you up for success. Well versed in adhering to industry standards like HIPAA, FDA 21 CFR Part 11, and GDPR, we are a custom healthcare software development company which knows how to build medical and healthcare applications that drive profitable outcomes.
Beyond the technology and compliances, we have a deep understanding of healthcare workflows. By relying on us, you will invest in a software solution that’s ready to tackle the complexities of healthcare delivery while staying compliant with regulations. Our healthcare solutions will allow you to successfully focus on your core mission: providing quality healthcare.
